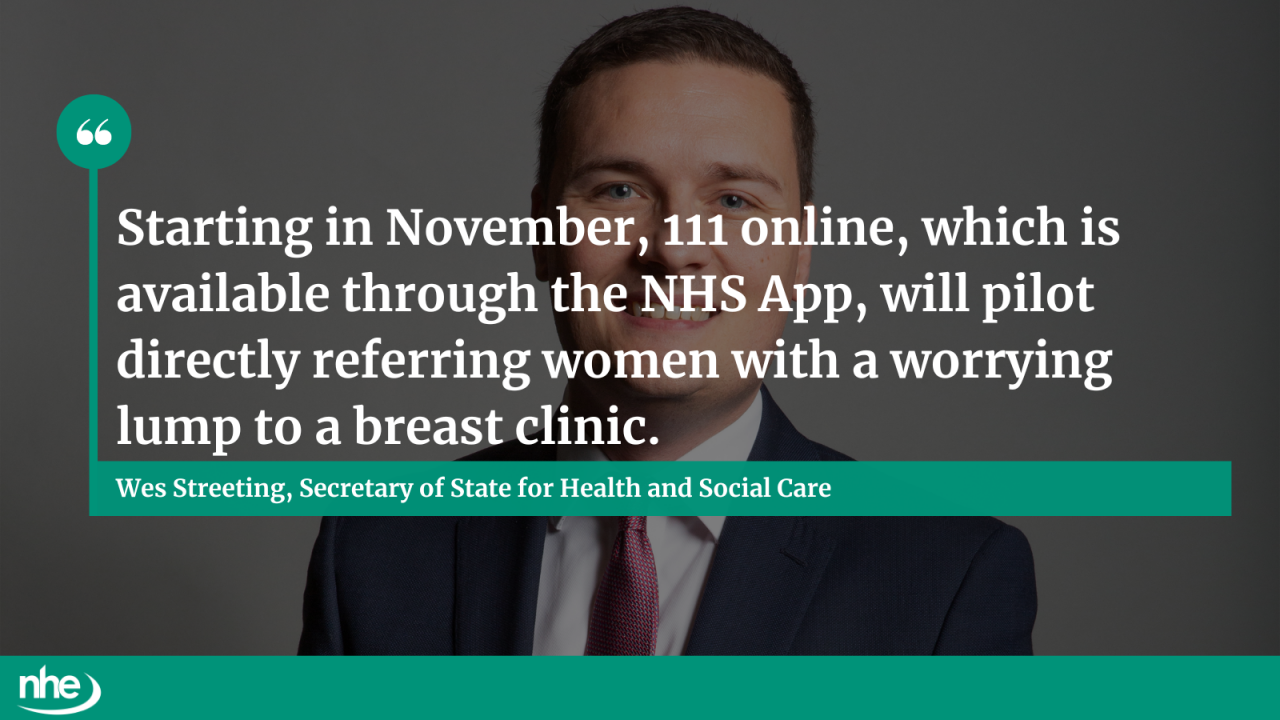
As part of a new expansion to the NHS App, women with worrying breast cancer symptoms will be able to receive a referral directly to a clinic – speeding up cancer diagnosis and freeing up GP appointments.
The move was confirmed by health secretary Wes Steeting during his speech at the Royal College of GPs’ conference in Liverpool, with the trial set to launch locally in Somerset next month. Referrals will take place via 111 online which is available through the NHS App.
Health leaders will evaluate the success of the project before a wider, national roll-out is commissioned.
“Starting in November, 111 online, which is available through the NHS App, will pilot directly referring women with a worrying lump to a breast clinic,” said Streeting.
“That means faster diagnosis for cancer patients.”
The move also represents “just the start” of the plans for the NHS App, according to NHS England’s transformation director, Dr Vin Diwakar.
The future through data
The upcoming 10-year reform plan for the NHS – informed by the recent Darzi Review – will heavily feature the development of single patient records, the health secretary also confirmed.
The Department of Health and Social Care intends to support more research through data, with NHSE being tasked with helping studies to harness the most out of the data collected from consenting patients.
The secretary of state added: “Patients have given their consent for their data to be shared with these studies. But we still see, far too often, that this data is not shared according to patients’ wishes.
“That’s why I am directing NHSE to take away this burden from you. Just like they did during the pandemic, if a patient explicitly consents to sharing their data with a study, NHSE will take responsibility for making this happen.”
This will be conducted with the “very highest” standards of data security. This will help better share data according to patients’ wishes.
The government has said the change will catalyse:
- new treatments;
- a bolstered life sciences industry; and
- an acceleration of the desired shift from sickness to prevention.
Unnecessary workload and bureaucracy
In a further bid to release GP time, as well as cut down on bureaucracy, the DHSC is launching the Red Tape Challenge, which will be led by NHSE’s Claire Fuller and Stella Vig – primary care medical director and medical director for secondary care and quality respectively.
The challenge will see GPs, hospitals and integrated care boards asked what works and what needs to be changed. This feedback will then be reviewed by a group of doctors across primary and secondary care.
Responding to the speech, RCGP’s chair, Professor Kamila Hawthorne, said: "It's encouraging that he is listening and has taken heed of what we have asked for in our manifesto to free up GPs to spend more time with patients through cutting red tape - GPs go into the profession to care for patients, not to fill in forms.
“Our members say they're spending a third of their time on unnecessary workload and bureaucracy.”
Image credit: iStock