Patients visiting their GP practice can expect more support than ever before, thanks to thousands of new healthcare staff working in local communities and the new GP access recovery plan.
More than 31,000 additional staff have been recruited into healthcare roles at general practices across the country since 2019. This expanded team of health professionals includes pharmacists, mental health practitioners, paramedics, physios, and social prescribers.
The NHS is now raising awareness of the support available from these community health teams, which are now available in every part of the country. This is important because record numbers of people are seeking support from their family doctors, but with one in five GP appointments for non-medical reasons, the NHS wants to make sure that the right help is available.
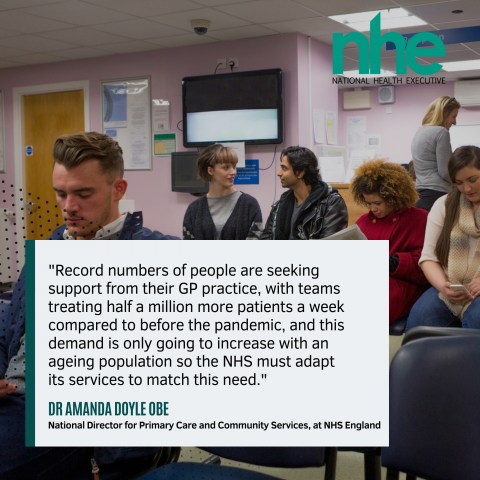
Patients can still see their GP if they need to, but the NHS is training more than 7,500 staff to better assess patients' needs when they first contact their practice so they can be seen by the right health professional. For example, if a patient has muscular pain, they will be booked straight into see a physiotherapist.
This expansion of support services at GP practices is part of the NHS's plan to improve access to care and reduce the pressure on GPs. The NHS is also making it easier for people to contact their GP with the NHS app, which has been used by 32 million people to book appointments or receive test results.
Public awareness of the range of support available at GP practices remains low. A new survey has revealed that one in three people in England are unaware of the different options available to them. However, the survey also found that more than two in three people were happy to receive care from another health worker, recognising they didn't always need to see a GP.
Tens of thousands of people are now receiving help from expanded social prescribing teams every month for non-medical issues. This can include support getting back into the workplace through volunteering, or involvement in community projects to address loneliness.
Social prescribing has been shown to be a low-cost intervention that can help people to manage their own health better, now and in the long term. It also helps to free up family doctors' time for patients who need their care and treatment.
Health minister Neil O'Brien said: "For most of us, general practice is our front door to the NHS and this is why we're expanding the support on offer to patients. There's now an extra 31,000 professionals – such as dieticians, paramedics and physiotherapists – working as part of GP teams and providing vital care to patients, or supporting doctors and nurses to do so. GPs delivered about 15% more appointments over the last year compared to pre-pandemic, and that's the result not just of more staff, but the hard work of teams in general practice."
Rachel Power, chief executive of the Patients Association, said: “We welcome this information campaign and the expansion of services available to patients in primary care.
“Enabling patients to receive care from different health professionals in the familiar surroundings of their general practice will suit many patients. But they need to know what services are available and how they fit in with the more familiar professionals such as the GP and practice nurse.”
Photo: iStock